
Nico Dosenbach, MD, PhD
Associate Professor, WashU Neurology
- Phone: 314-454-6006
- Email: dosenbachn@nospam.wustl.edu
Understanding use-driven brain network plasticity in children with brain injury, in order to develop novel neurorehabilitative treatments
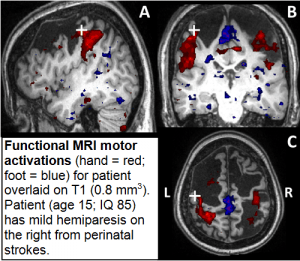
The goal of our research is to understand use-driven brain network plasticity in children with brain injury, in order to develop novel neurorehabilitative treatments. To this end, we are studying childrens’ brains using resting state functional connectivity MRI (rs-fcMRI) and task-based functional MRI (fMRI). We are focused on pushing structural and functional MRI acquisition and analysis methodology to the level of individual patients. In order to create and annotate the connectomes of individuals (‘Individuomes’) we must first improve the signal-to-noise, spatial resolution and replicability of fMRI and rs-fcMRI data. High-fidelity ‘Individuomes’ should help accelerate fMRI-based diagnostics and neurofeedback rehabilitation therapy.
One of the main complications for rs-fcMRI and fMRI in children is excessive head movement, which introduces systematic distortions. Post-hoc data censoring methods can remove movement artifact from rs-fcMRI data, but in children post-hoc censoring leads to extremely high data loss rates. In order to decrease the time and resources required for pediatric fMRI research we are developing a real-time head motion monitoring system called FIRMM (fMRI Integrated Real-time Motion Monitor) in collaboration with Dr. Fair at Oregon Health Sciences University. FIRMM will allow scan operators to adjust the scanning paradigm based on a participant’s head movement. FIRMM will also be used to train children to keep their heads still while in the MRI scanner, using real-time feedback.
In collaboration with Drs. Petersen, Schlaggar, Nelson, Greene and McDermott we are working on custom data-acquisition, spatial registration and statistical approaches for single subject analyses. Functional MRI processing pipelines tailor-made for single subjects will further improve our ability to characterize functional brain networks in individuals.
In order to find new treatments for children with brain injury, we must also find ways to relate underlying brain network changes to changes in behavior. Traditional means for assessing developmental progress and behavior in children are often biased, time-consuming and unreliable. Therefore, with support from Dr. Lang’s research group, we have heavily invested in wearable biosensors (accelerometers) that allow us to accurately measure limb movement in children with brain injury, as well typically developing children.
We are currently conducting a multi-modal MRI study of Constraint-Induced Movement Therapy (CIMT) together with Ranken Jordan Hospital. The study is benefiting from our recent methodological advances in motion monitoring, single-subject analyses and accelerometry. CIMT requires children with hemiplegia to have their more functional upper extremity immobilized in a cast for three weeks, while undergoing intense 1:1 occupational therapy daily. Our study repeatedly evaluates children with brain injury before and after CIMT in order to identify brain network changes that correlate with improved post-treatment motor function.