A team of researchers led by diabetes specialists and biomedical engineers at Washington University School of Medicine in St. Louis and Cornell University has demonstrated that, using a miniscule device, they can implant insulin-secreting cells into diabetic mice. Once implanted, the cells secrete insulin in response to blood sugar, reversing diabetes without requiring drugs to suppress the immune system.
The findings are published June 2 in the journal Science Translational Medicine.
“We can take a person’s skin or fat cells, make them into stem cells and then grow those stem cells into insulin-secreting cells,” said Jeffrey R. Millman, PhD, an associate professor of medicine at Washington University and one of the study’s co-senior investigators. “The problem is that in people with Type 1 diabetes, the immune system attacks those insulin-secreting cells and destroys them. To deliver those cells as a therapy, we need devices to house cells that secrete insulin in response to blood sugar, while also protecting those cells from the immune response.”
In previous research, Millman, also an associate professor of biomedical engineering, developed and honed a method to make induced pluripotent stem cells, and to then grow those stem cells into insulin-secreting beta cells. Millman previously used those beta cells to reverse diabetes in mice, but it was not clear how the insulin-secreting cells might safely be implanted into people with diabetes.
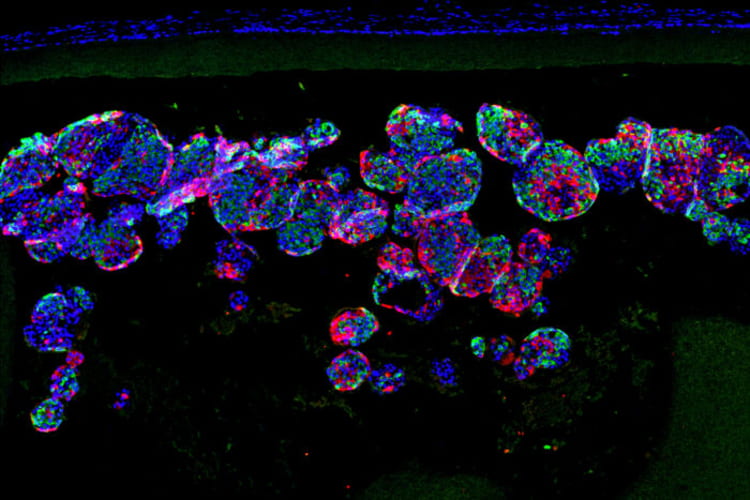
“The device, which is about the width of a few strands of hair, is micro-porous — with openings too small for other cells to squeeze into — so the insulin-secreting cells consequently can’t be destroyed by immune cells, which are larger than the openings,” said Millman. “One of challenges in this scenario is to protect the cells inside of the implant without starving them. They still need nutrients and oxygen from the blood to stay alive. With this device, we seem to have made something in what you might call a Goldilocks zone, where the cells could feel just right inside the device and remain healthy and functional, releasing insulin in response to blood sugar levels.”